We Can't Pour From Empty Cups: Why We Demand Guaranteed Uninterrupted Breaks
As nursing staff we race from room to room, checking vital signs, administering medications, and documenting everything. Our stomachs growl and it's been eight hours since breakfast, but the call lights are relentless, and a new admission just rolled in. Hopefully we will get time to eat later.
This isn't just one bad day. For many of us, it's every day.
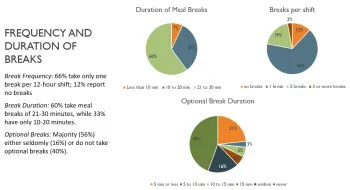
Recently I conducted a project on one of our hospital's acute care units to understand why so many healthcare workers struggle to take breaks during 12-hour shifts. What I found wasn't surprising to those of us on the frontlines, but the numbers are still surprising: Two-thirds of the staff on this unit managed to take only one break in 12 hours, while a whopping twelve percent took no breaks.
Let that sink in. In what other profession would we accept working half a day without stopping to eat, rest, or even use the bathroom?
Burnout Isn't Just a passing phenomenon
We've all heard about healthcare worker burnout. Sometimes you can hear the collective eyes roll when administration presents us with another "wellness initiative" involving meditation apps or yoga classes. But burnout isn't just feeling tired or stressed — it's a recognized occupational syndrome that happens when job demands consistently outstrip our resources.
The pandemic pushed healthcare workers to a breaking point. In fact, 62% of providers worldwide reported high burnout during the height of the pandemic, according to a cross-sectional study by Gambaro et al. (2023). But even before COVID, the cracks were showing. Now, burnout costs the U.S. healthcare system $9 billion annually just in nurse turnover according to a report from the HHS.
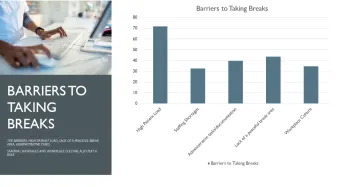
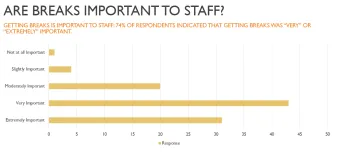
When I surveyed staff on a unit at our hospital about what prevents them from taking breaks, the answers were revealing:
- 72% cited high patient loads.
- 44% pointed to inadequate break environments.
- 40% blamed administrative duties.
- 35% said workplace culture made them feel guilty for taking breaks.
"Breaks tend to be treated as a luxury, not a necessity," one nurse commented. Another said, "Even when I do get a break, I'm still carrying the phone or pager, so I get called back before I can even finish my meal."
Does any of this sound familiar?
Shifting Some Responsibility Away From Individuals and Demanding More from the Hospital
For years, we've been told that managing burnout is our personal responsibility. Be even more resilient than you already are. Just practice self-care! Do yoga! Meditate! Here is another pizza party!
But research is confirming what we already know: burnout isn't a personal failing — it's a system failure.
A major study of over 15,000 nurses found that when asked what would help most with burnout, nurses didn't ask for meditation apps or resilience training. They wanted structural changes: better staffing, uninterrupted breaks, improved team communication, and less paperwork.
As one researcher said, we're "not suffering from a yoga deficiency." We're suffering from systems that don't prioritize our basic human needs.
What Actually Works
Based on my research and a deep dive into the literature, I've identified four solutions that make a real difference:
First, dedicated break coverage. Hospitals that implement "break nurses" or buddy systems — where someone is specifically responsible for covering patients while staff take breaks — see measurable reductions in burnout. This isn't rocket science: when nurses know their patients are covered, they can truly disconnect from their duties during breaks.
Second, a cultural shift. When managers and charge nurses actively encourage breaks — not just in theory but in practice — staff feel permitted to take them. The unit where my project took place had a supportive manager who took implementing practice into reality seriously. He made rounds and offered help. He started taking breaks with his staff, showing them that he didn’t see it as a luxury, but as something that is necessary and that they’re entitled to it.
Third, better break spaces. Where we take breaks really matters. One study found that nurses who took breaks in a garden showed significantly better burnout scores than those stuck in windowless break rooms. Quiet, comfortable spaces away from call bells and monitors make breaks restorative. The unit manager where my project was implemented remodeled their breakroom based on staff feedback.
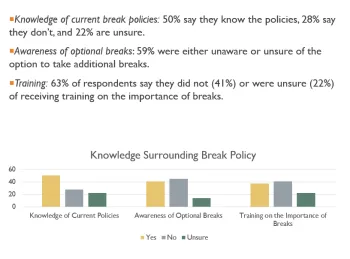
Fourth, clear break policies. Nearly half of the nurses I surveyed didn't even know they were entitled to additional breaks beyond their meal break. When policies are clear and consistently enforced, break-taking becomes normalized, even encouraged.
What Our Union Can Do
This is where we come in as a union. While individual hospitals decide how to allocate resources, we have collective power to demand changes that benefit both nurses and patients.
The financial case is clear: hospitals with burnout reduction programs spend about $5,000 less per nurse annually than those maintaining the status quo. Over five years, hospitals turn over an average of 102.6% of their RN workforce — meaning they essentially replace their entire staff and then some. Each percentage point of turnover costs an additional $262,500.
Union organizing around breaks should focus on:
- Negotiating for adequate staffing ratios that allow for break coverage.
- Establishing guaranteed, uninterrupted break periods.
- Creating dedicated break relief positions.
- Improving break room environments.
- Developing break policies that recognize rest as essential, not optional.
- Not punishing us when we are unable to get a break.
When hospitals push back citing costs, we need to remind them of the math: preventing burnout is cheaper than addressing its consequences.
Our Understanding and Expectations
Taking breaks isn't self-indulgent — it's self-preservation. And it's not just about us. Rested nurses provide safer care. Period.
When we are exhausted and hungry, we are not the people we want to be. That's not a personal failing — it's human physiology.
The right to rest during long shifts isn't a perk or a privilege. It's a necessity for safe patient care. And it's time our healthcare systems recognized that.
Our union is fighting for these changes because we believe in both our well-being and in delivering safer care. Because the truth is, we can't pour from empty cups — and no one should ask us to try.
Real Results: What Happens When Hospitals Take Breaks Seriously
These aren't just theories. On this particular unit where they implemented my recommendations, the results were almost immediate.
After presenting leadership with a strategic plan focusing on breaks, they quickly made changes: renovating break rooms to create more inviting spaces, implementing a consistent "lunch buddy" system to ensure coverage, providing education about burnout prevention, and establishing monthly tracking reports to maintain accountability.
The numbers tell the story: Before implementation, the unit averaged 212 missed lunches monthly. Within just one month, missed lunches decreased by approximately half. By February, only 78 lunches were missed — the lowest level in over two years.
But the most impressive changes the unit manager detailed weren’t statistical. He reported increased morale among staff, with more laughter and smiling, even amid high patient acuity. Staff now better understand the connection between taking breaks and reducing burnout.
This is what happens when hospitals shift from treating breaks as an optional monetary headache to recognizing them as essential. And this is exactly what our union aims to achieve for all our members.
Why This Matters to Me
As a frontline nurse, I've experienced firsthand the difference that a well-designed break system makes. In my unit, we have dedicated staff who come in at staggered times specifically to provide lunch relief before they are rotated into patient care. This system ensures we receive not just our meal breaks but also those optional fifteen-minute breaks that so many nurses don't know they're entitled to.
Beyond the dedicated relief staff, our charge nurses actively coordinate coverage, helping us watch each other's patients when needed. This Swiss cheese approach means taking a break isn't just theoretically possible — it's an expected part of our day.
The contrast is stark when I speak with colleagues who worked at Union hospitals. Many friends who have transitioned to union facilities with guaranteed, protected breaks report much lower stress levels, higher job satisfaction and better work life balance. A common theme was that many didn't realize how much more rested they felt every day until they worked somewhere that treated breaks as everyday working procedures rather than an optional luxury.
Union hospitals that negotiate guaranteed breaks consistently show higher morale. It's not just about the breaks themselves — it's what they represent: a workplace that acknowledges nurses are human beings with basic needs, not just task-performing machines.
Breaks shouldn’t be a paradox where we are punished if we can’t take one. And that’s precisely why our union is fighting for structured systems that support us. We know from experience that when breaks are guaranteed through collective bargaining rather than left to chance, everyone benefits: nurses, hospitals, and most importantly, our patients.
We Can't Pour From Empty Cups: Why We Demand Guaranteed Uninterrupted Breaks
